Abstract
Objective: Early detection of sarcopenia using accessible screening tools is essential but challenging due to the limitations of current instruments. The purpose of this study was to validate the Mini Sarcopenia Risk Assessment (MSRA-7 and MSRA-5) questionnaires in Turkish.
Methods: A total of 157 community-dwelling older adults were consecutively recruited from an outpatient geriatric clinic. Muscle strength and mass were measured using handgrip strength, chair stand test, and bioelectrical impedance analysis. Since only one participant met the criteria for confirmed sarcopenia, analyses focused on probable sarcopenia as defined by the European Working Group on Sarcopenia in Older People (EWGSOP2). Reliability was assessed with Cronbach’s alpha and intraclass correlation coefficients (ICCs). Construct validity was evaluated via Spearman correlation with the SARC-F questionnaire. Diagnostic performance was analyzed using ROC curves.
Results: The Turkish MSRA-7 and MSRA-5 demonstrated acceptable internal consistency (Cronbach’s alpha: 0.650 and 0.705, respectively) and excellent reliability (ICC range: 0.971–0.992). Both versions showed strong negative correlations with SARC-F (r = -0.767 for MSRA-7; r = -0.781 for MSRA-5, p < 0.001), confirming construct validity. ROC analysis yielded AUC values of 0.688 for MSRA-7 and 0.721 for MSRA-5. The MSRA-5 showed slightly superior diagnostic accuracy.
Conclusion: The Turkish adaptations of the MSRA-7 and MSRA-5 demonstrate validity and reliability as instruments for screening probable sarcopenia. Given its stronger internal consistency and diagnostic performance, in clinical practice, the MSRA-5 could be the preferred tool for early identification and intervention in older adults in Türkiye.
Keywords: older adults, sarcopenia, screening tool
Main Points
- The Turkish versions of the Mini Sarcopenia Risk Assessment (MSRA-7 and MSRA-5) questionnaires demonstrated acceptable validity and excellent reliability for screening sarcopenia among older adults.
- The MSRA-5 version showed slightly better internal consistency and diagnostic performance compared to MSRA-7, suggesting it may be the preferred tool for clinical practice in Türkiye.
- Strong negative correlations with the SARC-F questionnaire support the construct validity of the Turkish MSRA versions, and newly identified cut-off points enhance their applicability in the Turkish older population.
Introduction
Sarcopenia, defined as the progressive loss of muscle mass and function with aging, is a serious public health issue associated to higher risks of falls, frailty, functional decline, and mortality.1 Despite its clinical significance, no universal consensus exists on its diagnostic criteria or cut-off points. Several international organizations, including the European Working Group on Sarcopenia in Older People (EWGSOP2)2, have proposed criteria emphasizing muscle strength along with assessment of skeletal muscle mass (SMM).
However, these diagnostic methods are often inaccessible in routine clinical practice, contributing to the underdiagnosis of sarcopenia. To address this, simple screening tools have been developed, such as the Strength, Assistance with walking, Rise from a chair, Climb stairs, and Falls (SARC-F) questionnaire.3 Despite its widespread use, the SARC-F questionnaire has been shown to have low sensitivity, which may result in a substantial number of sarcopenia cases being overlooked. In the Turkish validation study by Bahat et al., SARC-F demonstrated sensitivity values ranging between 25% and 50 %, depending on the diagnostic criteria applied, further highlighting its limitations in reliably identifying individuals at risk.4
Rossi et al. developed the Mini Sarcopenia Risk Assessment (MSRA) questionnaire to enhance screening accuracy, achieving a sensitivity of 80.4% and a specificity of 60.4%.5 The MSRA questionnaire is available in two formats: MSRA-7 and MSRA-5. The original MSRA-7 version consists of seven items assessing key risk factors for sarcopenia, including age, weight loss, level of physical activity, mobility limitations, recent hospitalization and protein intake (via questions on dairy and meat consumption). Each item is scored with weighted values, yielding a total score ranging from 0 to 40, where lower scores indicate higher risk for sarcopenia. The shortened MSRA-5 version omits the two nutrition-related items (dairy and meat intake), resulting in a 5-question tool with a total score range from 0 to 60. In both versions, cut-off values have been established to differentiate individuals at risk, allowing for rapid, non-invasive screening in clinical and community settings.
The MSRA questionnaire has been validated in multiple languages, including Thai, Polish, Spanish, Greek, Brazilian Portuguese, and Chinese, underscoring its cross-cultural applicability.6-11 Given Türkiye’s aging population and the increasing prevalence of sarcopenia, a validated Turkish version is essential. The objective of this study is to translate, culturally adapt, and validate the MSRA questionnaire for Turkish-speaking older adults, ensuring its effectiveness in clinical and research settings. Establishing a reliable screening tool will aid early intervention and improve health outcomes for older individuals in Türkiye.
Materials and Methods
Subjects
The study participants were community-dwelling older individuals aged 65 and above, recruited from an outpatient Geriatrics clinic. Demographic information, including participants’ age, sex, and level of education was recorded. Furthermore, all participants had a comprehensive geriatric assessment, which encompassed evaluations of functional status with the Katz Index of Independence in Activities of Daily Living12,13, Lawton Brody Instrumental Activities of Daily Living scale14,15, Clinical Frailty Scale (CFS)16, depressive symptoms via the Yesavage Geriatric Depression Scale (YDS)17,18, nutritional status with the Mini Nutritional Assessment–Short Form (MNA-SF)19,20, cognitive function measured by Standardised Mini-Mental State Examination (SMMSE)21, and sarcopenia screening with SARC-F3,4 and Turkish versions of MSRA.
Exclusion criteria included the existence of severe cognitive impairment, acute illnesses or exacerbations of chronic diseases requiring hospitalization, severe hearing or visual impairments preventing accurate questionnaire completion, and refusal to participate. All participants provided informed consent prior to enrollment. The study protocol was approved by the local ethics committee of Hacettepe University Health Sciences Research Ethics Committee (Reference number GO 21/644) and conducted in accordance with the Declaration of Helsinki.
Translation and adaptation process
Permission for the use of the MSRA has been obtained from Dr. Andrea P. Rossi, corresponding author of the original study.5 The translation and cultural adaptation of the MSRA-7 and MSRA-5 questionnaires into Turkish were performed following standardized international guidelines for cross-cultural adaptation of health-related measures. Initially, the MSRA questionnaires were independently translated into Turkish by two bilingual experts. The two translations were compared, and discrepancies were resolved by consensus, resulting in a single forward-translated Turkish version. Subsequently, this version underwent backward translation into English by two independent translators unfamiliar with the original questionnaire. The backward-translated versions were compared with the original questionnaires to ensure consistency and equivalency. A panel of experts, reviewed the translations for cultural appropriateness and relevance. After minor modifications, including changing the term ‘milk coffee’ to ‘tea or coffee’ to align with Turkish cultural preferences and removing the term ‘ragout’ due to the absence of an equivalent Turkish word, the Turkish versions were pretested with a sample of older adults (n=16) for clarity and comprehensibility, resulting in the final Turkish MSRA questionnaires (Appendix).
Reliability
Internal consistency reliability was assessed using Cronbach’s alpha. Inter-rater reliability was evaluated by comparing questionnaire results from two independent raters who assessed the same participants (n=16) on the same day. Intra-rater reliability (test-retest reliability) was measured by having the same rater administer the questionnaire to the same participants with an interval of approximately two weeks. Both inter-rater and intra-rater reliabilities were analyzed using ICCs, with values ≥0.75 indicating excellent reliability.
Measurement of muscle strength and muscle mass
Handgrip strength was assessed using a calibrated handheld dynamometer (T.K.K.5401; Takei Scientific Instruments). Participants performed the measurement three times for the dominant hand, and the highest recorded value (kg) was used. Muscle strength was additionally assessed through the chair stand test, measuring the time (seconds) taken to rise from a chair five consecutive times without arm support. Skeletal muscle mass was evaluated by bioelectrical impedance analysis (BIA) using a validated device (Bodystat QuadScan 4000). Skeletal muscle mass index (SMMI) was calculated by dividing appendicular skeletal muscle mass by height squared (kg/m²).
According to the Revised European Working Group on Sarcopenia in Older People (EWGSOP2) criteria, sarcopenia is defined as the presence of reduced muscle strength (HS <27 kg in men, <16 kg in women or chair stand test >15 s) combined with low muscle mass (<7 kg/m² for men and <5.5 kg/m² for women). Probable sarcopenia is identified when low muscle strength is detected.2 Since only one participant met the EWGSOP2 criteria for confirmed sarcopenia, all analyses in this study were conducted based on the presence or absence of probable sarcopenia, which reflects reduced muscle strength without confirmed low muscle mass.
Statistical analyses
Descriptive statistics were presented as median (interquartile range [IQR]) for non-normally distributed continuous variables, mean ± standard deviation (SD) for normally distributed continuous variables, and frequencies and percentages (%) for categorical variables. Comparisons between groups were performed using t-test or Mann-Whitney U tests for continuous variables, where appropriate and Chi-square tests for categorical variables. Construct validity was evaluated using Spearman correlation coefficients between the Turkish MSRA versions and SARC-F questionnaire. Receiver operating characteristic (ROC) curve analysis was performed to determine optimal cut-off points, sensitivity, and specificity for predicting probable sarcopenia. All statistical analyses were performed using SPSS version SPSS 25.0 (IBM Corp., Armonk, NY) with statistical significance set at p<0.05.
Results
A total of 157 participants (64.3% women) with a median age of 72 (68-78) were included in the study. Significant sex differences were observed in several demographic and clinical characteristics (Table 1). Women had notably lower education levels (87.1% ≤5 years vs. 48.2% in men, p<0.001), higher prevalence of hypertension (80.2% vs. 64.3%, p=0.028), lower prevalence of cardiovascular diseases (16.8% vs. 39.3%, p=0.002), and higher body mass index (BMI) (median BMI: 29.70 vs. 27.40 kg/m², p<0.001). Regarding components of comprehensive geriatric assessment, women showed slightly lower independence in activities of daily living as measured by the Katz and Lawton-Brody scales. Additionally, women had significantly higher YDS and CFS scores, and lower MNA-SF and SMMSE scores, and physical performance parameters such as handgrip strength and chair stand test scores. Women also scored higher in sarcopenia screening tools (SARC-F, MSRA-7, MSRA-5) and had lower skeletal muscle mass index (SMMI) values compared to men. However, no significant difference was found between sexes in the prevalence of probable sarcopenia.
| BMI: Body mass index, CFS: Clinical Frailty Scale, MNA-SF: Mini Nutritional Assessment Short Form, MSRA-5: Mini Sarcopenia Risk Assessment 5 items, MSRA-7: Mini Sarcopenia Risk Assessment 7 items, SARC-F: Strength, assistance with walking, rise from a chair, climb stairs and falls, SMMI: Skeletal Muscle Mass Index, SMMSE: Standardised Mini-Mental State Examination, YDS: Yesavage Geriatric Depression scale. Results were shown as mean ± 2SD for parametric variable (SMMI), median (IQR) for non-parametric variables (Age, BMI, Katz, Lawton-Brody, YDS and MNA-SF, CFS, SMMSE, handgrip strength, chair stand test, SARC-F and MSRA scores), and as numbers (n) and percentiles (%) for categorical variables. | |||
| Table 1. Demographic and clinical characteristics of the study population | |||
|
|
|
|
|
| Age |
|
|
|
| Education time | |||
| ≤ 5 years |
|
|
|
| > 5 years |
|
|
|
| Hypertension |
|
|
|
| Diabetes mellitus |
|
|
|
| Cardiovascular Disease |
|
|
|
| Cerebrovascular Disease |
|
|
|
| BMI (kg/m2) |
|
|
|
| Katz |
|
|
|
| Lawton Brody |
|
|
|
| YDS |
|
|
|
| MNA-SF |
|
|
|
| CFS |
|
|
|
| SMMSE |
|
|
|
| Handgrip strength (kg) |
|
|
|
| Chair stand test (s) |
|
|
|
| SARC-F |
|
|
|
| MSRA-7 |
|
|
|
| MSRA-5 |
|
|
|
| SMMI (kg/m2) |
|
|
|
| Probable Sarcopenia |
|
|
|
Reliability
Cronbach’s alpha was used to evaluate the internal consistency of the Turkish MSRA questionnaires, which demonstrated acceptable reliability with values of 0.650 for MSRA-7 and 0.705 for MSRA-5. Additionally, both inter-rater and intra-rater (test-retest) reliability were evaluated using ICCs. For MSRA-7, ICC was 0.983 (95% CI: 0.953–0.994) for inter-rater reliability and 0.992 (95% CI: 0.977–0.997) for intra-rater reliability. Similarly, MSRA-5 showed high reliability with ICC values of 0.971 (95% CI: 0.921–0.990) for inter-rater reliability and 0.988 (95% CI: 0.967–0.996) for intra-rater reliability. These findings indicate excellent reliability of the Turkish versions of the MSRA questionnaires.
Construct validity
To evaluate the construct validity of the Turkish versions of MSRA-7 and MSRA-5, Spearman correlation analyses were conducted using the SARC-F questionnaire as a comparator. Strong negative correlations were found between SARC-F and both MSRA-7 (r = -0.767, p < 0.001) and MSRA-5 (r = -0.781, p < 0.001), indicating excellent construct validity of the Turkish MSRA questionnaires.
Cut-off values
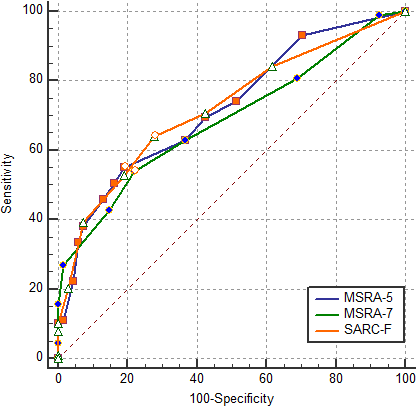
ROC curve analyses were conducted to determine the diagnostic performance of MSRA-7, MSRA-5, and SARC-F questionnaires in predicting probable sarcopenia. The areas under the ROC curve (AUC) were 0.688 (95% CI: 0.609–0.759, p<0.001) for MSRA-7 (Figure 1), 0.721 (95% CI: 0.644–0.790, p<0.001) for MSRA-5 (Figure 2), and 0.723 (95% CI: 0.646–0.791, p<0.001) for SARC-F (Figure 3).
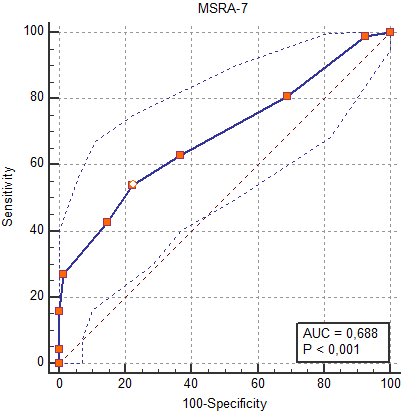
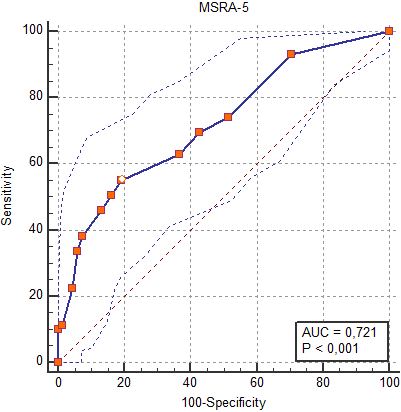
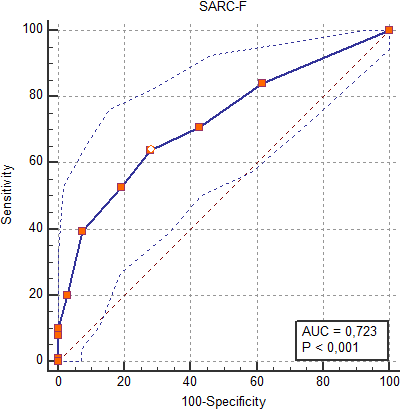
The optimal cut-off points identified using the Youden index were ≤20 for MSRA-7 (sensitivity: 53.93%, specificity: 77.94%), ≤35 for MSRA-5 (sensitivity: 55.06%, specificity: 80.88%), and ≥3 for SARC-F (sensitivity: 64.04%, specificity: 72.06%).
Pairwise comparisons of ROC curves revealed no statistically significant differences between MSRA-5, MSRA-7, and SARC-F (MSRA-5 vs MSRA-7, MSRA-5 vs SARC-F, and MSRA-7 vs SARC-F; p=0.08, p=0.95, p=0.28, respectively.) (Figure 4). These findings suggest that all three tools have comparable diagnostic performance for screening probable sarcopenia, with MSRA-5 and SARC-F demonstrating slightly higher overall accuracy compared to MSRA-7.
Discussion
The objective of this study was to translate, culturally adapt, and validate the Turkish versions of the MSRA-7 and MSRA-5 questionnaires for the screening of sarcopenia in community-dwelling older adults in Türkiye. Our findings exhibited acceptable validity and excellent reliability of both Turkish MSRA versions, consistent with previous validation studies in other populations and languages.
In the original validation by Rossi et al., MSRA displayed a sensitivity of 80.4% and specificity of 60.4% for detecting sarcopenia risk among older Italian adults.5 In our study, MSRA-5 exhibited a sensitivity of 55.06% and specificity of 80.88%, whereas MSRA-7 had slightly lower sensitivity (53.93%) and specificity (77.94%). Also, the MSRA-7 version demonstrated a relatively lower Cronbach’s alpha (0.650) compared to MSRA-5 (0.705), suggesting moderate internal consistency. This discrepancy may be partly attributed to the question regarding dairy product consumption in the MSRA-7, which may have introduced variability in participant responses. In the Turkish context, cultural dietary habits, such as variability in types and frequency of dairy intake may lead to inconsistencies in how older adults interpret and respond to this item. The MSRA-5 version notably omits this question, concentrating instead on fundamental risk factors including age, weight loss, physical activity, and hospitalizations. This more streamlined structure appears to contribute to its stronger internal consistency and better overall diagnostic performance in our study, as reflected by both higher Cronbach’s alpha and superior ROC curve characteristics (AUC: 0.721 vs. 0.688 for MSRA-7).
Comparing our results with other cross-cultural validation studies, consistent trends emerge in favor of the MSRA-5 questionnaire over MSRA-7 in terms of diagnostic accuracy. In the Chinese validation conducted by Yang et al., MSRA-5 was shown to be more effective than MSRA-7 for sarcopenia screening in community-dwelling older adults, aligning with our own findings.11 Similarly, the Polish validation reported high sensitivity for both MSRA-7 and MSRA-5, however, MSRA-5 demonstrated better specificity compared to MSRA-7.7 In the Spanish validation study, MSRA-5 again showed superior diagnostic performance compared to MSRA-7.8 Taken together, these validation studies support the notion that MSRA-5’s more concise structure—focusing on core sarcopenia risk factors such as age, mobility, weight loss, comorbidities, and recent hospitalization—may contribute to its superior diagnostic utility across diverse populations. Our study confirms this pattern in Turkish older adults, further reinforcing the MSRA-5 as a culturally adaptable and clinically effective tool for sarcopenia screening.
Despite the known limitations of the SARC-F questionnaire, particularly its low sensitivity for detecting sarcopenia22, it was selected as the reference tool for evaluating construct validity in this study due to its widespread clinical use and endorsement by international guidelines. Specifically, the EWGSOP2 recommends SARC-F as a first-line screening tool in clinical practice.2 Its use across diverse healthcare settings and populations provides a practical benchmark for comparison with newly validated instruments like the MSRA. Therefore, the strong negative correlations observed between SARC-F and both MSRA-7 and MSRA-5 further support the construct validity of the Turkish versions of MSRA within a real-world clinical screening context. The results align with those observed in the earlier cross-cultural validation study by Pantouvaki et al., where strong inverse correlations were found between MSRA-7 and MSRA-5 scores and the SARC-F (r = -0.741 and r = -0.724, respectively; p < 0.001).9
The optimal cut-off points identified in our study (≤20 for MSRA-7 and ≤35 for MSRA-5) differ slightly from those reported in the original Italian validation and other language adaptations. For example, Rossi et al. proposed ≤30 for MSRA-7 and ≤45 for MSRA-5, reflecting differences in population characteristics and sarcopenia prevalence.5 The lower thresholds observed in the Turkish population may be attributed to cultural and dietary habits, differing healthcare access, or variations in the interpretation of specific questionnaire items, such as those related to mobility and protein intake. These findings underscore the significance of validation tailored to specific contexts and emphasize the need to establish culturally appropriate cut-off points to optimize the diagnostic accuracy of sarcopenia screening tools across diverse settings.
However, several limitations should be noted. Firstly, our study utilized BIA for muscle mass measurement, which, although practical, is less precise than imaging techniques like dual-energy X-ray absorptiometry (DXA). This limitation may influence the accuracy of sarcopenia diagnosis. Secondly, our analyses were conducted solely on patients with probable sarcopenia, as only one participant was identified with confirmed sarcopenia based on EWGSOP2 criteria. This limitation could restrict the applicability of the findings to confirmed sarcopenia cases and highlights the need for future studies to include a larger number of individuals diagnosed with confirmed sarcopenia. Additionally, our study was conducted in a single outpatient setting, potentially limiting the generalizability of findings to broader community or institutional populations. Finally, although our sample size was statistically adequate, larger multi-center studies could further validate these results and explore subgroup differences more comprehensively.
Conclusion
In conclusion, the Turkish versions of the MSRA-7 and MSRA-5 questionnaires exhibit strong psychometric properties for screening sarcopenia among older adults. The MSRA-5, with its slightly better diagnostic performance, could be recommended as the preferred screening tool in clinical practice. Their use can facilitate early identification and intervention strategies in clinical and research settings within Türkiye, ultimately contributing to better geriatric care outcomes.
Ethical approval
This study has been approved by the Hacettepe University Health Sciences Research Ethics Committee (approval date 26.05.2021, number GO:21/644). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Sayer AA, Cooper R, Arai H, et al. Sarcopenia. Nat Rev Dis Primers. 2024;10:68. https://doi.org/10.1038/s41572-024-00550-w
- Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16-31. https://doi.org/10.1093/ageing/afy169
- Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14:531-532. https://doi.org/10.1016/j.jamda.2013.05.018
- Bahat G, Yilmaz O, Kılıç C, Oren MM, Karan MA. Performance of SARC-F in regard to sarcopenia definitions, muscle mass and functional measures. J Nutr Health Aging. 2018;22:898-903. https://doi.org/10.1007/s12603-018-1067-8
- Rossi AP, Micciolo R, Rubele S, et al. Assessing the risk of sarcopenia in the elderly: the Mini Sarcopenia Risk Assessment (MSRA) questionnaire. J Nutr Health Aging. 2017;21:743-749. https://doi.org/10.1007/s12603-017-0921-4
- Akarapornkrailert P, Muangpaisan W, Boonpeng A, Daengdee D. Validation of the Thai version of SARC-F, MSRA-7, and MSRA-5 questionnaires compared to AWGS 2019 and sarcopenia risks in older patients at a medical outpatient clinic. Osteoporos Sarcopenia. 2020;6:205-211. https://doi.org/10.1016/j.afos.2020.11.006
- Krzymińska-Siemaszko R, Deskur-Śmielecka E, Styszyński A, Wieczorowska-Tobis K. Polish translation and validation of the Mini Sarcopenia Risk Assessment (MSRA) questionnaire to assess nutritional and non-nutritional risk factors of sarcopenia in older adults. Nutrients. 2021;13:1061. https://doi.org/10.3390/nu13041061
- Moreno-Sánchez I, Aibar-Almazán A, Carcelén-Fraile MD, et al. Cross-cultural adaptation and clinical validation of the mini sarcopenia risk assessment questionnaire in community-dwelling spanish older adults. Diagnostics (Basel). 2024;14:2123. https://doi.org/10.3390/diagnostics14192123
- Pantouvaki A, Kastanis G, Patelarou E, Alpantaki K, Kleisiaris C, Zografakis-Sfakianakis M. Greek translation, cultural adaptation and validation of the mini sarcopenia risk assessment questionnaire, to evaluate sarcopenia in Greek elderly at a hospital setting. Nurs Rep. 2023;13:404-411. https://doi.org/10.3390/nursrep13010037
- Ribeiro LS, Souza BG, de Lima JB, Pimentel GD. Cross-cultural adaptation of the Brazilian Portuguese-translated version of the Mini Sarcopenia Risk Assessment (MSRA) questionnaire in cancer patients. Clin Pract. 2021;11:395-403. https://doi.org/10.3390/clinpract11020054
- Yang M, Hu X, Xie L, et al. Validation of the Chinese version of the mini sarcopenia risk assessment questionnaire in community-dwelling older adults. Medicine (Baltimore). 2018;97:e12426. https://doi.org/10.1097/MD.0000000000012426
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919. https://doi.org/10.1001/jama.1963.03060120024016
- Arik G, Varan HD, Yavuz BB, et al. Validation of Katz index of independence in activities of daily living in Turkish older adults. Arch Gerontol Geriatr. 2015;61:344-350. https://doi.org/10.1016/j.archger.2015.08.019
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-186.
- Işık EI, Yılmaz S, Uysal I, Basar S. Adaptation of the lawton instrumental activities of daily living scale to Turkish: validity and reliability study. Ann Geriatr Med Res. 2020;24:35-40. https://doi.org/10.4235/agmr.19.0051
- Özsürekci C, Balcı C, Kızılarslanoğlu MC, et al. An important problem in an aging country: identifying the frailty via 9 Point Clinical Frailty Scale. Acta Clin Belg. 2020;75:200-204. https://doi.org/10.1080/17843286.2019.1597457
- Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37-49. https://doi.org/10.1016/0022-3956(82)90033-4
- Durmaz B, Soysal P, Ellidokuz H, Işık AT. Validity and reliability of geriatric depression scale-15 (short form) in Turkish older adults. North Clin Istanb. 2018;5:216-220. https://doi.org/10.14744/nci.2017.85047
- Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin Geriatr Med. 2002;18:737-757. https://doi.org/10.1016/s0749-0690(02)00059-9
- Sarikaya D, Halil M, Kuyumcu ME, et al. Mini nutritional assessment test long and short form are valid screening tools in Turkish older adults. Arch Gerontol Geriatr. 2015;61:56-60. https://doi.org/10.1016/j.archger.2015.04.006
- Molloy DW, Alemayehu E, Roberts R. Reliability of a standardized mini-mental state examination compared with the traditional mini-mental state examination. Am J Psychiatry. 1991;148:102-105. https://doi.org/10.1176/ajp.148.1.102
- Kera T, Kawai H, Hirano H, et al. Limitations of SARC-F in the diagnosis of sarcopenia in community-dwelling older adults. Arch Gerontol Geriatr. 2020;87:103959. https://doi.org/10.1016/j.archger.2019.103959
Copyright and license
Copyright © 2025 The author(s). This is an open-access article under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.