Abstract
Objective: This study aimed to identify demographic characteristics associated with nutritional risk and evaluate the prevalence and severity of malnutrition among adult patients admitted to the emergency department.
Methods: This cross-sectional study included 187 adult emergency department patients with stable vital signs and a Glasgow Coma Scale score greater than 13. Malnutrition risk and status were assessed using the Nutritional Risk Screening-2002 (NRS-2002) and Subjective Global Assessment (SGA) within the first 24 hours of hospital admission. Data were collected through structured bedside interviews.
Results: According to NRS-2002, 24.6% of patients were at risk for malnutrition, while SGA identified moderate malnutrition in 41.3% (SGA-B) and severe malnutrition in 39.1% (SGA-C) of cases. Binary logistic regression analysis showed that increasing age was significantly associated with nutritional risk (OR=1.032; 95% CI: 1.008–1.056; p=.008). Gender and reason for emergency admission did not reach statistical significance.
Conclusion: This study highlights that malnutrition risk is substantial among emergency department patients and significantly associated with increasing age. These findings emphasize the importance of incorporating systematic nutritional screening protocols at emergency admission, particularly in older adults, to ensure timely dietetic assessment and optimize clinical outcomes.
Keywords: clinical nutrition, emergency department, malnutrition, nutritional risk screening
Main Points
- Approximately one in four adult patients presenting to our tertiary emergency department (ED) were at nutritional risk according to NRS-2002 (≥3).
- Logistic regression analysis identified increasing age as a statistically significant independent predictor of nutritional risk.
- Emergency admissions due to respiratory, neurological, gastrointestinal, or infectious diseases were not significantly associated with increased nutritional risk in this cohort.
- The model demonstrated good fit and modest predictive strength.
- These findings support routine use of nutritional screening tools like NRS-2002 in emergency departments, particularly for elderly patients, to enable early dietetic intervention and potentially improve patient outcomes.
Introduction
Malnutrition is a universal public health problem that can be seen all over the world at all ages and is also an impediment to global poverty eradication, productivity, and economic growth.1 This perspective is further supported by the World Health Organization, which emphasizes the serious and enduring consequences of the global malnutrition problem on individuals, families, communities, and nations, including developmental, economic, social, and medical impacts.2
The term “malnutrition” includes a range of conditions characterized by a lack, excess, or imbalance of various essential nutrients, which can result in negative impacts on the body’s composition, functioning, and clinical outcomes.3 While it is possible for malnourished individuals to experience either undernutrition or overnutrition, the term “malnutrition” is frequently used interchangeably with “undernutrition”.
Malnutrition is an under-recognized and undertreated condition that affects 30–50% of hospitalized patients.3,4 A research investigation was conducted in Türkiye involving a total of 34 hospitals located in 19 cities, with a sample size of 29,139 patients. The study revealed that 15% of the patients exhibited signs of nutritional risk. The prevalence of nutritional risk was found to be highest among patients in the intensive care unit, with a rate of 52%. Additionally, a notable proportion of patients in the internal medicine department, specifically 16.4%, were identified as malnourished. The study results showed that a mere 51.8% of patients identified as having nutritional risk were provided with appropriate nutritional support.5 More than one-third (36%) of patients experience malnutrition before hospital discharge, a condition that can be prevented, and the prevalence of malnutrition increases with the length of hospital stay.6 This situation may occur as a result of diminished dietary consumption for a variety of reasons, including impaired absorption of macronutrients and/or micronutrients, heightened nutrient excretion, or modified metabolic requirements.3 When a patient admitted to the hospital for any reason is malnourished or in a state of disease, extensive changes occur in physiological function, which negatively affects the success of the treatment, prolongs the recovery period, catabolic metabolism, chronic low-grade inflammation, hospital stay, increases the risk of developing nosocomial infections, and causes increased rates of morbidity and mortality.3,7
In the malnutrition screenings performed on hospitalized patients in the world and in Türkiye, it has been shown that the frequency of malnutrition is higher in some clinics such as oncology, pulmonology, geriatrics, surgery, and intensive care units, and these clinics are evaluated as risky clinics in terms of malnutrition.5,8,9 Although emergency services are not included in these malnutrition screening studies, there are some studies in the literature in recent years emphasizing the frequency of malnutrition and its negative effects, especially in elderly patients who applied to the emergency department.10-12 In a limited number of studies examining the prevalence of malnutrition among adults presenting to emergency services, the prevalence ranged from 15 to 29%, particularly among elderly patients.12-14 Malnutrition screening is generally not performed on individuals who apply to the emergency department. However, screening for malnutrition in the emergency department can capture a vulnerable population that may be overlooked.10
The prevention and potential reversal of malnutrition can be achieved through the timely and sufficient implementation of nutritional therapy. Nevertheless, it is imperative to enhance the awareness and knowledge of healthcare providers, while also establishing clinical protocols, to effectively identify and address this issue.15 The identification of malnutrition has been proposed by the European Society for Clinical Nutrition and Metabolism (ESPEN) through a two-step methodology. The initial step entails utilizing a validated screening instrument, such as the Nutritional Risk Screening 2002 (NRS-2002), to evaluate the probability of malnutrition in individuals. Following that, a thorough assessment is performed utilizing the Subjective Global Assessment (SGA) in order to validate the diagnosis of malnutrition. Given that these tests do not necessitate any form of analysis, it can be inferred that there are no supplementary expenses involved.16 Following the assessment of an individual’s nutritional status, the provision of nutritional support should be administered by the dedicated nutritional support team, if deemed necessary. Nevertheless, there is a dearth of hospitals equipped with nutritional support teams, and their ability to offer emergency services is typically lacking.17
The aim of the research is to determine the prevalence of malnutrition among adult patients who are admitted to the emergency department. Additionally, the study aims to identify the specific patient population that is particularly susceptible to malnutrition as well as evaluate the severity of malnutrition in patients who are diagnosed with this condition. The research results suggest that there is a need for increasing awareness about the evaluation of nutritional status among patients admitted to the emergency department.
Methods
Study design and setting
This descriptive, cross-sectional study aimed to evaluate malnutrition status among adult patients admitted to the Ankara University Ibn-i Sina Hospital Emergency Department. The study included all adult patients (aged ≥18 years) presenting to the emergency department over one week. Patients were recruited consecutively throughout the week (24 hours/day) to ensure comprehensive inclusion.
Selection of participants
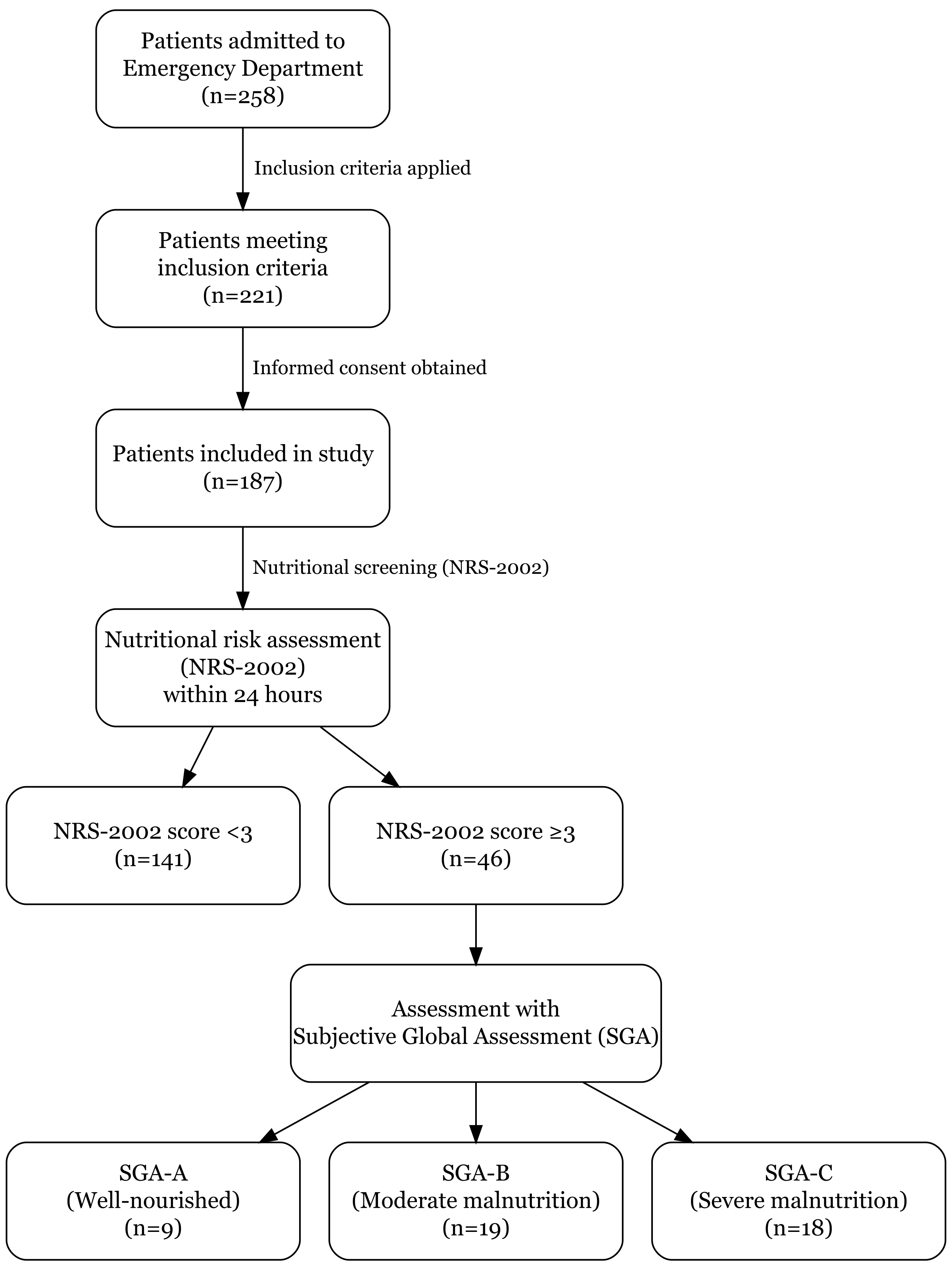
Detailed patient information was obtained from hospital patient files and interviews conducted with patients or their relatives. Patients with unstable vital functions, those who were uncooperative, disoriented, or had a Glasgow Coma Scale ≤13 were excluded due to potential unreliability in obtaining accurate information and difficulties in performing nutritional assessments. Eligible patients were informed about the research, and written informed consent was obtained from those agreeing to participate. A total of 187 adult patients who met these inclusion criteria and agreed to participate constituted the study sample. The study was conducted in March 2016. The flowchart illustrating the patient selection process is presented in Figure 1.
Sample size estimation
The sample size was evaluated retrospectively with G*Power version 3.1.9.7, indicating that with an effect size of 0.3 (medium), an alpha level of 0.05, and a statistical power of 0.80, the required minimum sample size was 143 patients. Therefore, the recruited sample of 187 patients is considered adequate for statistical reliability.
Methods and measurements
Data related to patient demographics (age, gender), reasons for emergency department visits, and comorbid conditions were collected through structured bedside interviews. Interviews were performed either directly with patients or, if necessary, their relatives. Weight change during the preceding three months was recorded as (a) documented weight in electronic medical records when available or (b) patient/relative self-report; only unintentional loss >5% body weight was accepted as clinically significant. Patients’ nutritional status data were collected using validated nutritional assessment tools (NRS-2002 and SGA).
The NRS-2002 and SGA questionnaires were used to assess each patient’s nutritional status and nutritional risk within the first 24 hours after admission. An ad hoc working group developed the NRS-2002 for the purpose of determining a person’s nutritional status, and the ESPEN was in charge of the group.18 This nutritional tool has been proven to have the capacity to correctly identify patient populations that stand to gain the greatest advantages from receiving nutritional support. It is necessary to begin by adding the “Nutritional Score” (0–3) to the “Severity of Disease Score” (0–3) before moving on to the next step of the calculation for the nutritional risk score. Patients who are 70 or older receive a score of 1, regardless of their gender. The highest possible score is seven. Per ESPEN guidance, an NRS-2002 total score ≥3 denotes nutritional risk warranting further assessment and intervention. Accordingly, patients who scored ≥3 proceeded to SGA for malnutrition grading, whereas those with a score <3 were considered low risk and did not undergo further nutritional assessment.
The Subjective Global Assessment (SGA) is a tool for nutritional assessment that was first introduced in 198219, and it has since been validated by controlled clinical trials.20,21 SGA is defined by the presence of five clinically significant characteristics related to nutritional status. These characteristics include decreased nutrient intake, inadvertent weight loss, oral intake-related symptoms, functional capacity, and metabolic demand. A physical examination is also part of the SGA, and during this examination, particular attention is paid to fluid accumulation, muscle atrophy, and subcutaneous fat loss. Individuals are either considered to be severely malnourished (SGA-C), mildly or moderately malnourished (SGA-B), or well-nourished (SGA-A).
Statistical analysis
IBM SPSS Statistics 22 (IBM Corp., Armonk, NY, USA) was used to analyze the study data. The Kolmogorov-Smirnov test was utilized to check the normal distribution of the variables. Categorical variables were examined using the Chi-squared (χ2) test and presented as frequency distributions. Binary logistic regression analysis was conducted to identify factors independently associated with nutritional risk (NRS-2002 ≥3 as the dependent categorical variable). The confidence interval was set at 95%, with a significance level of p<.05 in all statistical tests.
Ethical approval
Ethical approval for the study was obtained from the Ankara University Faculty of Medicine Clinical Research Ethics Committee (approval date May 11, 2015, number 08-344-15). At the beginning of the study, all participants provided informed consent by signing a consent form before participating in the study. The study was conducted following the principles outlined in the Declaration of Helsinki.
Results
The study comprised 187 patients in total, of which 52.4% were female and 47.6% were male. Of the patients, most (50.8%) were older than 65. In the previous three months, 25.1% of the patients had experienced weight loss. The majority (31.6%) of applications to the emergency room were for respiratory disorders. According to data obtained with the NRS-2002, 24.6% (n=46) of individuals were at risk of malnutrition. Among these 46 high-risk patients who underwent further assessment using the SGA tool, 41.3% were classified as moderately malnourished (SGA-B) and 39.1% as severely malnourished (SGA-C) (Table 1).
Table 2 shows the relationship between nutritional assessment scores (NRS-2002 and SGA) and demographic characteristics of the patients admitted to the emergency department. Patients aged ≥65 years were significantly more likely to have higher nutritional risk scores (NRS-2002 ≥3: 67.4%; p=.01) and severe malnutrition (SGA-C: 61.1%; p=.005). Similarly, recent weight loss within the last three months was strongly associated with increased nutritional risk (NRS-2002 ≥3: 72.3%; p<.001) and severe malnutrition (SGA-C: 72.2%; p<.001). However, no statistically significant association was found between nutritional assessment scores (NRS-2002 or SGA) and gender or reasons for emergency department admission (p>.05).
| Data are presented as observed counts (O), with expected counts (E) in parentheses: O (E). *Due to low frequencies, cardiovascular, endocrine, hematological, cancer, bone diseases, liver diseases, urinary system diseases, suicide, swelling, lassitude, and ear, nose, and throat diseases were merged under the category of "other medical conditions". αPearson’s Chi-squared (χ2) test. βFisher's exact test. p<.05. | ||||||||||||
| Table 2. The relationship between nutritional assessment scores (NRS-2002 and SGA) and demographic characteristics | ||||||||||||
| Characteristics |
|
|
|
|
||||||||
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|||
| Gender | ||||||||||||
| Male |
|
|
|
|
|
|
|
|
|
|
|
|
| Female |
|
|
|
|
|
|
|
|
|
|
||
| Age (year) | ||||||||||||
| 19-64 |
|
|
|
|
|
|
|
|
|
|
|
|
| ≥65 |
|
|
|
|
|
|
|
|
|
|
||
| Weight loss in the last 3 months | ||||||||||||
| Yes |
|
|
|
|
|
|
|
|
|
|
|
|
| No |
|
|
|
|
|
|
|
|
|
|
||
| Reasons for application to emergency department | ||||||||||||
| Respiratory diseases |
|
|
|
|
|
|
|
|
|
|
|
|
| Neurological diseases |
|
|
|
|
|
|
|
|
|
|
||
| Gastrointestinal diseases |
|
|
|
|
|
|
|
|
|
|
||
| Infections |
|
|
|
|
|
|
|
|
|
|
||
| Other medical conditions* |
|
|
|
|
|
|
|
|
|
|
||
| TOTAL |
|
|
|
|
|
|
|
|
|
|
||
Binary logistic regression analysis revealed that increasing age was significantly associated with nutritional risk (NRS-2002 ≥3) (OR=1.032; 95% CI: 1.008–1.056, p=.008). Gender and reasons for admission to the emergency department did not demonstrate statistically significant associations (p>.05). The overall regression model was statistically significant (χ²=17.879, df=6, p=.007), demonstrated good fit (Hosmer–Lemeshow χ²=11.795, p=.161), and explained 13.6% of the variance in nutritional risk (Nagelkerke R²=.136) (Table 3).
| Binary logistic regression analysis was performed. Dependent variable: Nutritional risk assessed by NRS-2002 (score ≥3 vs. <3). Nagelkerke R2=.136; Overall model: χ2=17.879, df=6, p<.007. Hosmer-Lemeshow test (χ2=11.795, p=.161). p<.05 statistically significant. The “reasons for application to emergency department” row reflects the omnibus test of the categorical variable as a whole. “Other medical conditions” was used as the reference category. B: regression coefficient; SE: standard error; OR (Exp(B)): odds ratio; CI: confidence interval. |
||||||
| Table 3. Factors associated with nutritional risk (NRS-2002 ≥3) in patients admitted to the emergency department | ||||||
| Variables |
|
|
|
|
|
|
| Age |
|
|
|
|
|
|
| Gender |
|
|
|
|
|
|
| Reasons for application to emergency department |
|
|
|
|
|
|
| Respiratory diseases |
|
|
|
|
|
|
| Neurological diseases |
|
|
|
|
|
|
| Gastrointestinal diseases |
|
|
|
|
|
|
| Infections |
|
|
|
|
|
|
| Other medical conditions |
|
|
|
|
|
|
Discussion
The results of this study highlight a significant prevalence of nutritional risk among adult patients admitted to the emergency department, with notable implications for clinical practice and healthcare management. Using the NRS-2002, 24.6% of all patients were classified as nutritionally at risk. Among the 46 patients with an NRS-2002 score ≥3 who subsequently underwent SGA, 19 (41.3%) were classified as moderate malnutrition (SGA-B) and 18 (39.1%) as severe malnutrition (SGA-C) (Table 1). These figures correspond to 10.2% and 9.6% of the entire study population, respectively. Thus, the apparently higher SGA percentages merely reflect the distribution within the high-risk subgroup rather than the whole cohort. Although the absolute prevalence estimates differ because the two tools were applied to different denominators, both instruments consistently identify a sizeable malnourished population, underscoring the need for standardized and sequential screening approaches in emergency-care settings.22
The prevalence of nutritional risk identified in this study aligns closely with findings from international studies, emphasizing a universal healthcare concern. Previous research conducted in emergency department populations has consistently demonstrated significant malnutrition risks, especially among elderly cohorts. For instance, a study conducted in Ireland reported malnutrition in 7.6% of elderly patients, with an additional 28% identified as being at nutritional risk.10 Similarly, evidence from the United States indicated a rising trend in the prevalence of malnutrition among older emergency department visitors, emphasizing the increasing importance of addressing malnutrition as a public health priority.23
Advanced age was significantly associated with increased nutritional risk (OR=1.032; 95% CI: 1.008–1.056; p=.008) (Table 3). This result is consistent with extensive literature documenting the vulnerability of elderly populations to nutritional deficiencies due to physiological changes, polypharmacy, chronic illnesses, and socioeconomic factors such as social isolation and economic instability.24 Therefore, routine nutritional screening and targeted interventions for elderly patients in emergency departments are crucial for improving clinical outcomes and reducing healthcare costs associated with malnutrition.
Interestingly, neither gender nor reasons for emergency admission demonstrated a significant association with nutritional risk in our cohort (p>.05) (Table 3). In contrast to our findings, the study by Ratsavong et al.25 suggests that gender differences and specific admission reasons are influential determinants of nutritional status. The absence of significant associations in our study may reflect the heterogeneity in clinical presentations and demographic compositions of emergency populations, highlighting the necessity for further context-specific research to clarify these relationships.
In our cohort, respiratory disorders were the most common reason for emergency department visits (31.6%), consistent with prior literature highlighting the high acute care burden of pulmonary conditions. Although respiratory diseases did not emerge as statistically significant predictors of nutritional risk in the multivariate model, their clinical relevance remains noteworthy. Chronic respiratory illnesses such as chronic obstructive pulmonary disease (COPD) are frequently associated with increased metabolic demands, systemic inflammation, and symptoms such as dyspnoea and anorexia, all of which contribute to nutritional depletion and muscle wasting. Additionally, COPD-related malnutrition has been linked to impaired respiratory muscle function, reduced fat-free mass, and diminished quality of life, reinforcing the importance of nutritional vigilance even in the absence of statistical associations.26,27
The clinical and economic consequences of malnutrition emphasize its importance as a healthcare priority. Malnutrition significantly increases morbidity and mortality, delays wound healing, and raises susceptibility to infections.28,29 Additionally, malnutrition profoundly impacts healthcare systems by increasing hospital stays, higher readmission rates, and escalating healthcare costs. Previous systematic reviews and meta-analyses have consistently reported extended hospital stays and increased mortality among malnourished patients, further reinforcing the need for robust nutritional management protocols in acute care settings.30,31
In light of these findings, the substantial prevalence of nutritional risk identified in this study calls for the systematic implementation of standardized nutritional screening protocols in emergency departments. Special attention should be directed toward elderly patients, particularly those who report recent unintentional weight loss during triage, even though weight loss did not remain an independent predictor in multivariate analysis. Comprehensive nutritional assessment strategies and timely, individualized nutritional interventions should become standard practices to enhance patient outcomes, optimize resource utilization, and ultimately improve the quality of emergency medical care.
Limitations
The study’s cross-sectional design and relatively small sample size constitute key limitations; therefore, causal relationships between malnutrition and adverse clinical outcomes cannot be established. Although a post-hoc power calculation confirmed that the total sample (n=187) provided >80% power to detect the predefined medium effect for the primary outcome, the available numbers were insufficient for robust subgroup analyses (e.g., by specific admission diagnosis, gender, or weight-loss status). Consequently, estimates within these subgroups should be interpreted with caution and cannot be generalized beyond this cohort. In addition, being a single-center investigation limits the generalizability of the findings to other settings or broader patient populations. Reliance on self-reported data may also have introduced recall bias for certain variables. Data were collected in 2016; however, the absence of substantive changes in screening protocols since then limits the risk of temporal bias.
Nutritional assessment was restricted to two widely used tools (NRS-2002 and SGA); inclusion of additional instruments or biochemical markers might have yielded deeper insights into nutritional status. Although the NRS-2002 was originally developed for hospitalized patients, its application in emergency settings has been endorsed by ESPEN, particularly due to its ease of use and rapid applicability. However, the subjective nature of disease severity assessment within the NRS-2002 may introduce variability depending on clinical judgment and individual clinician experience, especially under emergency conditions.
Moreover, patients with severe cognitive impairment or life-threatening trauma were excluded for pragmatic reasons; this underrepresentation of the sickest cohort may have led to an underestimation of true malnutrition prevalence.
Finally, downstream clinical outcomes such as length of stay, readmission, or in-hospital mortality were not collected, preventing correlation of nutritional risk with hard endpoints; future prospective work should address this gap.
Despite these limitations, our results underscore the critical importance of systematic malnutrition screening in emergency departments, particularly for elderly patients, because early recognition and timely nutritional interventions can enhance outcomes and reduce complications.
Conclusion
Our findings corroborate prior ED studies by confirming a high malnutrition risk, particularly among older adults, in a Turkish tertiary centre. These findings highlight the importance of early nutritional screening and timely interventions in emergency department settings. As one of the few studies exploring nutritional risk in Turkish emergency departments, our results emphasize the need for increased awareness and widespread implementation of systematic nutritional assessments to mitigate adverse clinical outcomes associated with malnutrition. Future research should focus on developing effective interventions, including tailored nutritional counseling and support, to address malnutrition risks in emergency patients.
Acknowledgements
The authors thank the medical and nursing staff at Ankara University Ibn-i Sina Hospital Emergency Department who contributed.
Ethical approval
This study has been approved by the Ankara University Faculty of Medicine Clinical Research Ethics Committee (approval date May 11, 2015, number 08-344-15). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Dukhi N. Global prevalence of malnutrition: evidence from literature. In: Imran M, Imran A, editors. Malnutrition. London: IntechOpen; 2020:1-16. https://doi.org/10.5772/intechopen.92006
- World Health Organization (WHO). Malnutrition. 2024. Available at: https://www.who.int/news-room/questions-and-answers/item/malnutrition(Accessed on Sep 28, 2024).
- Saunders J, Smith T. Malnutrition: causes and consequences. Clin Med (Lond). 2010;10:624-627. https://doi.org/10.7861/clinmedicine.10-6-624
- Sauer AC, Goates S, Malone A, et al. Prevalence of malnutrition risk and the impact of nutrition risk on hospital outcomes: results from nutritionDay in the U.S. JPEN J Parenter Enteral Nutr. 2019;43:918-926. https://doi.org/10.1002/jpen.1499
- Korfali G, Gündoğdu H, Aydintuğ S, et al. Nutritional risk of hospitalized patients in Turkey. Clin Nutr. 2009;28:533-537. https://doi.org/10.1016/j.clnu.2009.04.015
- van Vliet IM, Gomes-Neto AW, de Jong MF, Jager-Wittenaar H, Navis GJ. High prevalence of malnutrition both on hospital admission and predischarge. Nutrition. 2020;77:110814. https://doi.org/10.1016/j.nut.2020.110814
- Tang Z, Cai H, Cui Y. Influence of early postoperative feeding in gastrointestinal anastomotic fistula formation and healing time in rabbits. Biomed Res Int. 2018;2018:8258096. https://doi.org/10.1155/2018/8258096
- Tangvik RJ, Tell GS, Guttormsen AB, et al. Nutritional risk profile in a university hospital population. Clin Nutr. 2015;34:705-711. https://doi.org/10.1016/j.clnu.2014.08.001
- Güzel S, Keser A, Bayram İK. Risk of malnutrition in general surgical patients. J Health Sci Med. 2021;4:55-62. https://doi.org/10.32322/jhsm.823458
- Griffin A, O'Neill A, O'Connor M, et al. The prevalence of malnutrition and impact on patient outcomes among older adults presenting at an Irish emergency department: a secondary analysis of the OPTI-MEND trial. BMC Geriatr. 2020;20:455. https://doi.org/10.1186/s12877-020-01852-w
- Vivanti A, Isenring E, Baumann S, et al. Emergency department malnutrition screening and support model improves outcomes in a pilot randomised controlled trial. Emerg Med J. 2015;32:180-183. https://doi.org/10.1136/emermed-2013-202965
- Gentile S, Lacroix O, Durand AC, et al. Malnutrition: a highly predictive risk factor of short-term mortality in elderly presenting to the emergency department. J Nutr Health Aging. 2013;17:290-294. https://doi.org/10.1007/s12603-012-0398-0
- Pereira GF, Bulik CM, Weaver MA, Holland WC, Platts-Mills TF. Malnutrition among cognitively intact, noncritically ill older adults in the emergency department. Ann Emerg Med. 2015;65:85-91. https://doi.org/10.1016/j.annemergmed.2014.07.018
- Andersen AL, Nielsen RL, Houlind MB, et al. Risk of malnutrition upon admission and after discharge in acutely admitted older medical patients: a prospective observational study. Nutrients. 2021;13:2757. https://doi.org/10.3390/nu13082757
- Reber E, Gomes F, Vasiloglou MF, Schuetz P, Stanga Z. Nutritional risk screening and assessment. J Clin Med. 2019;8:1065. https://doi.org/10.3390/jcm8071065
- Cederholm T, Bosaeus I, Barazzoni R, et al. Diagnostic criteria for malnutrition - an ESPEN consensus statement. Clin Nutr. 2015;34:335-340. https://doi.org/10.1016/j.clnu.2015.03.001
- A.S.P.E.N. Practice Management Task Force , Delegge M, Wooley JA, et al. The state of nutrition support teams and update on current models for providing nutrition support therapy to patients. Nutr Clin Pract. 2010;25:76-84. https://doi.org/10.1177/0884533609354901
- Kondrup J, Allison SP, Elia M, Vellas B, Plauth M; Educational and Clinical Practice Committee; European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415-421. https://doi.org/10.1016/s0261-5614(03)00098-0
- Baker JP, Detsky AS, Wesson DE, et al. Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med. 1982;306:969-972. https://doi.org/10.1056/NEJM198204223061606
- Norman K, Pirlich M, Smoliner C, et al. Cost-effectiveness of a 3-month intervention with oral nutritional supplements in disease-related malnutrition: a randomised controlled pilot study. Eur J Clin Nutr. 2011;65:735-742. https://doi.org/10.1038/ejcn.2011.31
- Norman K, Kirchner H, Freudenreich M, et al. Three month intervention with protein and energy rich supplements improve muscle function and quality of life in malnourished patients with non-neoplastic gastrointestinal disease-a randomized controlled trial. Clin Nutr. 2008;27:48-56. https://doi.org/10.1016/j.clnu.2007.08.011
- Ferguson M, Capra S, Bauer J, Banks M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition. 1999;15:458-464. https://doi.org/10.1016/s0899-9007(99)00084-2
- Lanctin DP, Merced-Nieves F, Mallett RM, et al. Prevalence and economic burden of malnutrition diagnosis among patients presenting to United States emergency departments. Acad Emerg Med. 2021;28:325-335. https://doi.org/10.1111/acem.13887
- Kaur D, Rasane P, Singh J, et al. Nutritional interventions for elderly and considerations for the development of geriatric foods. Curr Aging Sci. 2019;12:15-27. https://doi.org/10.2174/1874609812666190521110548
- Ratsavong K, van Elsacker T, Doungvichit D, et al. Are dietary intake and nutritional status influenced by gender? The pattern of dietary intake in Lao PDR: a developing country. Nutr J. 2020;19:31. https://doi.org/10.1186/s12937-020-00545-9
- Keogh E, Mark Williams E. Managing malnutrition in COPD: a review. Respir Med. 2021;176:106248. https://doi.org/10.1016/j.rmed.2020.106248
- Collins PF, Yang IA, Chang YC, Vaughan A. Nutritional support in chronic obstructive pulmonary disease (COPD): an evidence update. J Thorac Dis. 2019;11:S2230-S2237. https://doi.org/10.21037/jtd.2019.10.41
- Martín-Sánchez FJ, Cuesta Triana F, Rossello X, et al. Effect of risk of malnutrition on 30-day mortality among older patients with acute heart failure in emergency departments. Eur J Intern Med. 2019;65:69-77. https://doi.org/10.1016/j.ejim.2019.04.014
- Munoz N, Litchford M, Cereda E. Nutrition and wound care. Phys Med Rehabil Clin N Am. 2022;33:811-822. https://doi.org/10.1016/j.pmr.2022.06.007
- Uhl S, Siddique SM, McKeever L, et al. Malnutrition in hospitalized adults: a systematic review. Rockville, MD: Agency for Healthcare Research and Quality; 2021.
- Kaegi-Braun N, Faessli M, Kilchoer F, et al. Nutritional trials using high-protein strategies and long duration of support show strongest clinical effects on mortality: results of an updated systematic review and meta-analysis. Clin Nutr ESPEN. 2021;45:45-54.
Copyright and license
Copyright © 2025 The author(s). This is an open-access article under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.