Abstract
Objective: The aim of this study was to assess the prevalence of dysphagia in neurological patients using the Turkish Eating Assessment Tool-10 (EAT-10) screening test. Dysphagia is common in neurovascular, neurodegenerative, and neuromuscular diseases.
Methods: Three hundred neurological patients [stroke, multiple sclerosis (MS), dementia, Guillain Barre Syndrome (GBS), cerebral palsy (CP), myastenia gravis (MG)] were evaluated using the Turkish EAT-10 test. Data were analysed using IBM SPSS21, and p<0.05 was considered significant.
Results: The mean EAT-10 score was 6.22, with 69% of patients classified as dysphagic. The prevalence of dysphagia was highest in MG (100%) and dementia (83.32%). The severity of dysphagia was greater in women and patients aged 65+ (p<0.001).
Conclusions: Dysphagia is common in neurological patients. Due to the cost and limitations of instrumental methods, the Turkish EAT-10 test is recommended as a practical and reliable alternative for screening. Women and people over 65 may be at higher risk for dysphagia.
Keywords: swallowing, neurological dysphagia, EAT-10
Main Points
- Orally fed patients can face significant challenges due to dysphagia symptoms.
- Dysphagia is often observed in neurological patients. Following a neurological diagnosis, patients can be rapidly screened for dysphagia using the Turkish EAT-10 test.
- Risk of dysphagia varies according to gender and age-related factors
Introduction
Swallowing is the is the process of transferring food from the mouth to the stomach. The swallowing function incvolves both voluntary and involuntary movements. In order for the swallowing function to occur safely, the muscles involved in the swallowing function must be able to produce the appropriate force and contract at the appropriate rate and sequence. To achieve this, processes must occur that ensure harmonious sensorimotor coordination. The anatomical structures involved in swallowing are also related to our breathing and speech. This situation increases the impact of swallowing on vital functions. Swallowing function is closely related to malnutrition, dehydration, choking and quality of life.1-3
Swallowing consists of oral, pharyngeal and oesophageal phases. While conscious and unconscious movements are combined in the oral phase, unconscious movements are more dominant in the pharyngeal and oesophageal phases. If the structures cannot safely perform the necessary activities in any phase of these three stages dysphagia, also known as swallowing disorder or difficulty swallowing may occurs. Dysphagia can develop due to anatomical problems and damage to areas related to swallowing in the cerebral cortex or neuromuscular transmission.4
Swallowing is a very sensitive neurological function and neurogenic dysphagia is a consequence of neurological diseases. Studies have shown that post-stroke dysphagia is associated with increased risk of mortality or dependency, pneumonia, decreased quality of life, prolonged hospital stay, and health care costs.5,6 Dysphagia may also accompany the neurodegeneration process in Parkinson’s patients with bulbar dysfunction. Dysphagia has been associated with malnutrition and aspiration pneumonia in Parkinson’s patients.7 In neurological autoimmune diseases such as multiple sclerosis (MS), myastenia gravis (MG) and Guillain-Barre Syndrome (GBS), dysphagia may develop due to involvement of yhe muscle, brainstem, neuromuscular junction and corticospinal tract.8
Causes such as decreased tongue control, failure of the swallow reflex, decreased laryngeal closure and sensory loss have been associated with swallowing problems in people with MS.9 In cerebral palsy (CP), a neurodevelopmental disorder, impaired neck and trunk stabilisation, muscle weakness and muscle strength imbalance may prevent effective swallowing.10 In patients with dementia, cumulative changes caused by age-related sensorimotor changes, loss of muscle mass and strength, and loss of connective tissue elasticity may lead to dysphagia.11 Determining the status dysphagia in the course of neurological diseases is important for managing the prognosis and complications of the disease. It is possible to encounter dysphagia with different aetiologies in the clinic. However, it is diffucult to assess dysphagia with objective tests because it requires specialised equipment and experts. On the other hand, the use of a test with proven validity and reliability, such as the Turkish EAT-10, is valuable for both immediate use and for detecting dysphagia. Although there are many studies on the Turkish EAT-10 test, its use for screening purposes in the clinic is not common. This study supports the use of the Turkish EAT-10 for clinical screening in patients with different neurological diagnoses. Our study aims to integrate the Turkish EAT-10 test into the clinical workflow in dysphagia screening so that dysphagia of different aetiologies can be directed to appropriate treatment and managed. Our study aims to raise awareness of dysphagia and will contribute to the literature in this direction.
Material and Method
For our study, demographic characteristics and the Turkish EAT-10 questionnaire were applied to patients diagnosed with stroke, MS, dementia, GBS, CP, MG based on medical history, clinical examination and laboraty findings (magnetic resonance imaging, electroencephalography, electromyography) in neurological outpatient clinics and neurological intensive care units. The study design was cross-sectional and prevalence-based. We conducted our study between May 2022 and October 2022. Ethical approval for the study was obtained from the Non-invasive Ethics Committee of Dicle University, protocol number 301 dated 14.04.2022.
The EAT-10 questionnaire was used to determine the severity of oropharyngeal dysphagia and its validity and reliability were determined by Belafsky et al.12 In the EAT-10 test, translated into Turkish by Demir et al., each question is scored between ‘0’ (no problem) and ‘4’ (severe problem). The maximum possible total score is calculated as 40 points.13 According to the scoring of the test, a score of 3 or more is considered abnormal and the presence of dysphagia should be reported.14 The internal consistency of the Turkish EAT-10 was found to be high, with a Cronbach’s alpha value of 0.90 for test and 0.91 for test-retest repeatability; an alpha value of 0.70 to 0.80 indicates satisfactory consistency, 0.8 to 0.9 good consistency, and a value greater than 0.9 indicates excellent consistency.13 The sample consisted of patient from the neurology department, neurology intensive care unit patients and neurology outpatient clinic of Dicle University Hospital. For our study, we tried to determine the sample size by using the G-Power 3.1 package program. Accordingly, the study was planned to include a minimum of 200 patients, according to the power analysis performed with a type I error of 0.05, power of 0.80 and effect size of 0.20. Given the missing data, the study was stopped when data were collected from a total of 300 participants.
There was no gender discrimination in the people who participating in the study. As the questions of the EAT-10 test used in the study consist of questions related to swallowing experience, only orally fed individuals were included in the study. In the analysis of the results, the mean ± standard deviation, median, minimum and maximum values were used for the numerical results of the descriptive statistics. The distributions of grouped measurements were assessed using the normality test. Mann-Whitney U test and Kruskal-Wallis test were used to detect differences in numerical results. Values with p<0.05 were considered statistically significant.
Criteria for inclusion of volunteers in research:
- 18 years old or over 18 years old
- Oral feeding
- Have one of the following diagnoses; stroke, Parkinson’s disease, MS, dementia, GBS, CP, MG
- The volunteer for the study
- Have the cognitive ability to answer the survey questions
Exclusion criteria:
- Feeding by nasogastric (NG) Tube, percutaneous endoscopic gastrostomy (PEG) or percutaneous endoscopic jejunostomy (PEJ)
- History of laryngeal surgery
- History of chemotherapy/radiotherapy to the head and neck
- Having at a cognitive level that prevents you from answering survey questions
- Not volunteering for the study
These exclusions were made to ensure the validity of the survey responses, as the Turkish EAT-10 test requires patient participation and understanding and may not be applicable in these populations. In addition, as the data collection tool measured patient-perceived dysphagia based on swallowing experience, patients who were not fed orally could not be included.
Data collection
Patients were informed of the study. After verbal and written informed consent was obtained, a survey form was completed with demographic information about the patient. This form collected baseline information about the patient, including name, age, gender, medical diagnosis, body mass index (BMI), and dietary information. The EAT-10 Swallowing Function Screening Test form was explained to the patient as a swallowing assessment tool, the questions were asked one at a time, and the patient was asked to rate his or her dysphagia from 0 to 4 points for each question, with increasing severity.
Data analysis
Demographic information and EAT-10 data of the patients were analyzed using the IBM SPSS21 package. Mann-Whitney-U test and Kruskal-Wallis test were used to analyse the data for independent group means. Results were presnted as arithmatic mean±standard deviation. p<0.05 was considered significant. Normality: Mean ± standard deviation, median, minimum and maximum values were used for numerical results of descriptive statistics in the analysis of the results. The distributions of grouped measurements were assessed using the normality test. Mann-Whitney U test and Kruskal-Wallis test were used to detect differences in numerical outcomes that were not normally distributed. Values with p<0.05 were considered statistically significant.
Results
Of the patients who participated in the study, 52% were male. 47.5% of the patients participating in the study were 65 years or older (Table 1). 75.7% of patients in the study had a neurological diagnosis of less than one year. 10% of neurological patients in the study repoted having a history of pneumonia during the course of their illness (Table 2).
| Table 1. Demographic characteristics | |
| Demographic Category | Number |
| Gender (Female) | 144 |
| Gender (Male) | 156 |
| Age (18-64) | 157 |
| Age (65+) | 143 |
| Table 2. Medical history | |
| Medical Category | Number |
| Pneumonia Positive | 30 |
| Pneumonia Negative | 270 |
| Diagnosis <1 year | 227 |
| Diagnosis ≥ 1 year | 73 |
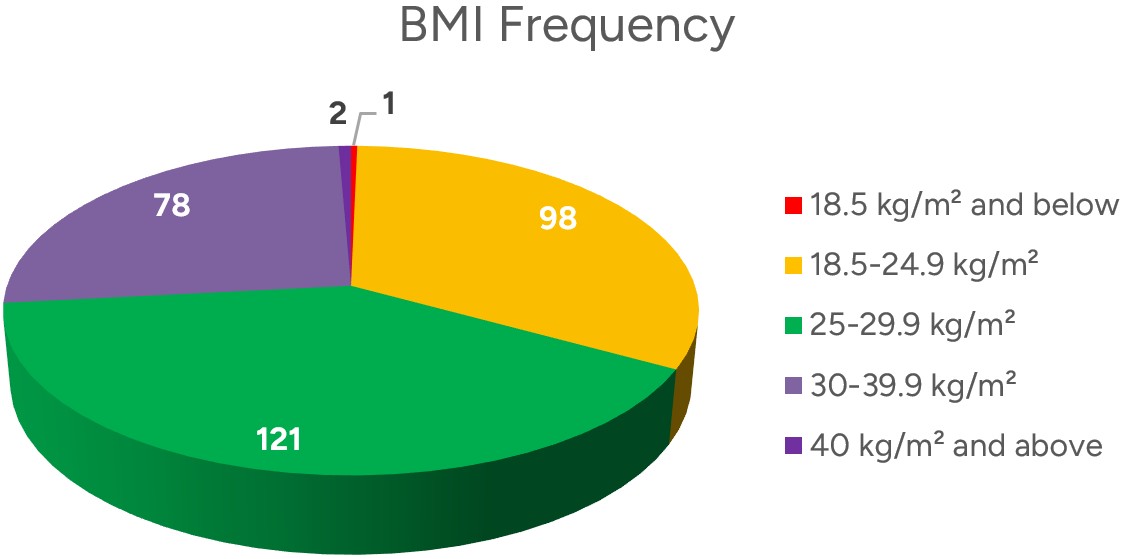
When the body mass indexes of the patients included in the study were calculated, 0.3% were underweight (18,5 kg/m2 and below), 32.6% were normal weight (18,5-24,9 kg/m2), 40.3% were overweight (25-29,9 kg/m2), 26% were obese (30-39,9 kg/m2), 0.7% were morbidly obese (40 kg/m2) (Figure 1).
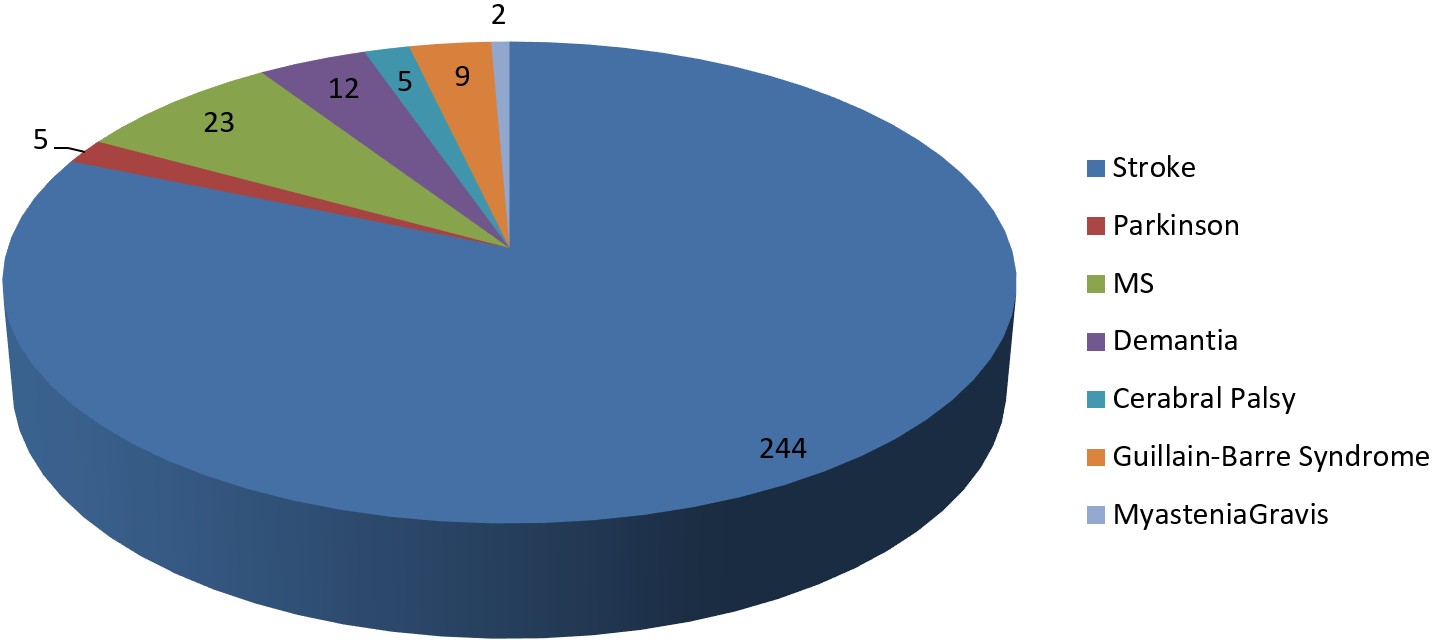
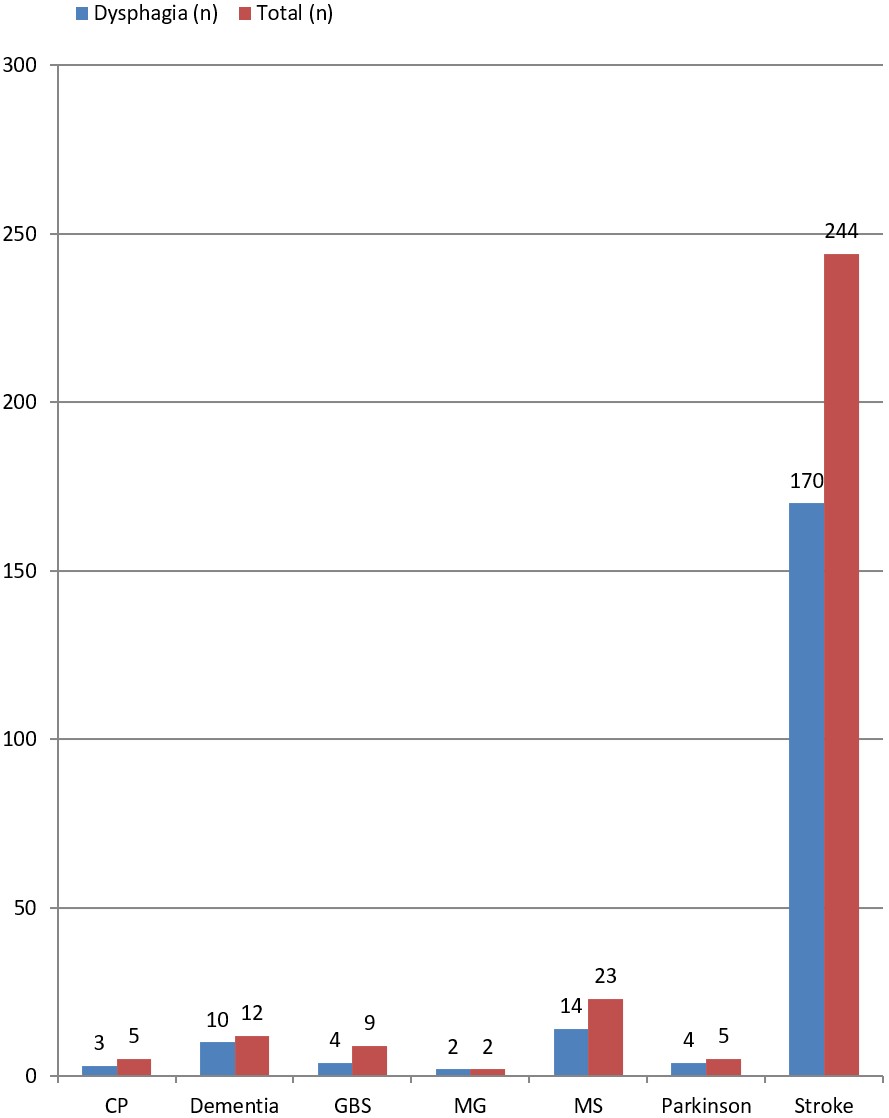
Our study includes a diverse cohort of neurological patients with conditions such as stroke, MS, Parkinson’ disease, dementia, Guillain-Barre syndrome, CP and MG (Figure 2). The prevalence of dysphagia within these subgroups provides valuable, under-researched insights into specific patient populations.
According to the assessment 69.67% of stroke patients; 80% of Parkinson’s patients; 60.8% of MS patients; 83.32% of dementia patients; 60% of CP patients; 44.4% of GBS patients; 100% of MG patients included in the study were in the dysphagia group (Figure 3). Since a score of 3 or more on the EAT-10 Test is considered abnormal, 69% of the patients scored within the abnormal range. The item with the highest score in the survey was “I have difficulty swallowing solid food”, while the item with the lowest score was “I feel pain when swallow”.
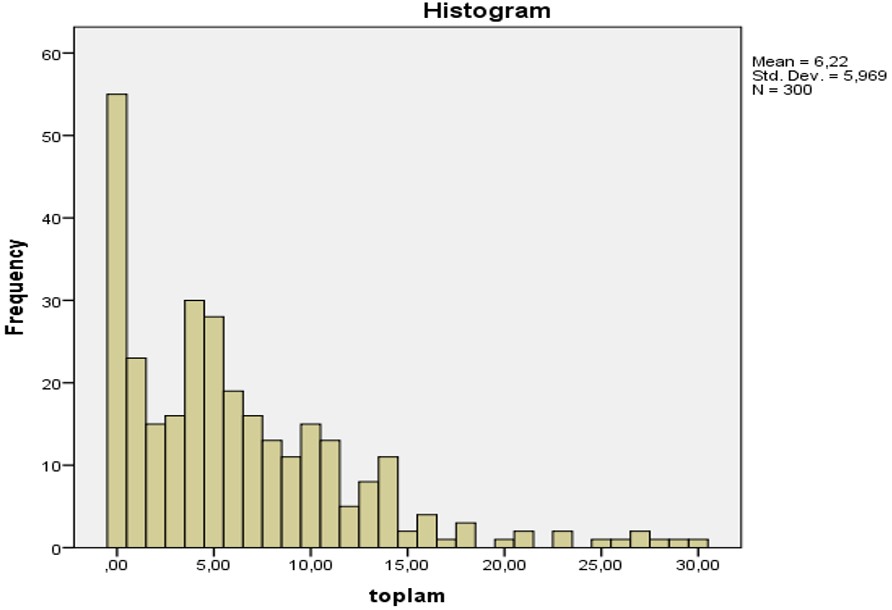
Changes in the patients’ responses to the survey according to demographic characteristics were analysed using the IBM SPSS21 package. According to the results of the normality test applied to the data, it was determined that the data were not normally distributed (Figure 4)
According to the non-parametric test results, the perceived severity of dysphagia was statistically significantly higher in women and those over 65 years of age (p<0.05). According to the test results, the time of neurological diagnosis and history of pneumonia were not statistically significantly associated with perceived dysphagia severity (p>0.05) (Table 3).
| Table 3. Mann-Whitney U Test for responses to the T-EAT-10 Test according to variables such as gender, age, history of pneumonia, and time of diagnosis | |||
|
|
|
|
|
|
Gender Female Male |
|
|
|
|
Age 18-64 65 and over |
|
|
|
|
Pneumonia History Positive Negative |
|
|
|
|
Time of Diagnosis <1 year 1 years and above |
|
|
|
There was no statistically significant difference in the severity of dysphagia as perceived by the test questions according to the patients’ body mass index (p>0.05) (Table 4).
| Table 4. T-EAT-10 test Kruskal-Wallis test result table according to BMI variable | ||||
|
|
|
|
|
|
| BMI Groups |
|
|
||
| Within Groups |
|
|
|
|
| Total | ||||
As the majority of the sample in our study consisted of stroke patients, we also performed statistical calculations specifically for stroke. According to the normality test performed on the results obtained from the data of the stroke patients, we found that the data were not normally distributed. We therefore used non-parametric tests. 69.7% of the stroke patients were classified as dysphagic because they scored 3 or more points on the Turkish EAT-10 test. According to the data collected from the stroke patients, the severity of dysphagia perceived by the patients was statistically significantly higher in women and participants over 65 years of age (p<0.05). The severity of dysphagia perceived by the stroke patients did not show a statistically significant difference according to the time of diagnosis of the disease, the patients’ history of pneumonia, and the patients’ body mass index (p>0.05) (Table 5 and Table 6).
| Table 5. Mann-Whitney U test for responses to the T-EAT-10 test according to variables such as gender, age, history of pneumonia and time of diagnosis of stroke patients | |||
|
|
|
|
|
|
Gender Female Male |
|
|
|
|
Age 18-64 65 and over |
|
|
|
|
Pneumonia History Positive Negative |
|
|
|
|
Time of Diagnosis <1 year 1 years and above |
|
|
|
| Table 6. Table of responses given by stroke patients to the T-EAT-10 test according to the Kruskal-Wallis test results according to the BMI variable | ||||
|
|
|
|
|
|
| BMI Groups |
|
|
||
| Within Groups |
|
|
|
|
| Total | ||||
Discussion
Dysphagia associated with malnutrition15 and pneumonia16 is an important and current problem. Our study used the Turkish EAT-10 test, a non-invasive assessment tool, with attention to contact isolation in accordance with pandemic conditions. The gold standards in the literature for the evaluation of dysphagia are the flexible endoscopic swallowing study and videofluoroscopic evaluation. In the literature, flexible endoscopic swallowing study and videofluoroscopy evaluation have been found to be statistically significantly associated with the EAT-10 test.17,18 It has become very difficult to use the methods used as the gold standard for assessing dysphagia, which require appropriate equipment and expert support, especially due to the measures brought about by the pandemic conditions. In our study, it was practical and facilitating to use the EAT-10 test, which has known validity and reliability, to assess and manage dysphagia under pandemic conditions. Despite the pandemic conditions, it is believed that the sample size of our study and the diverse cohort of patients included will contribute to the literature.
As 69% of the neurogenic patients participating in the study scored within abnormal limits, they were defined as dysphagic according to the survey results. In the study by Andrade et al., dysphagia screening was carried out on all patients in hospital wards and a prevalence of 10.5% was found in adults and elderly people. Since the group of neurological patients was not specifically selected in this study, it can be said that the rate was low compared to our study.19 In the study conducted by Abdulmassih et al. to evaluate the development of dysphagia in neurological patients during hospitalisation, 39 patients who were fed orally and in good clinical condition were included and evaluated by videofluoroscopy. The study found that 14 patients had mild dysphagia, 16 patients had moderate dysphagia and 9 patients had severe dysphagia, and the prevalence of dysphagia was 100%.20 It can be said that the detection rate may be higher if the study is conducted using objective and sensitive tests such as videofluoroscopy. It has been estimated in the literature that neurogenic dysphagia develops in 400,000 to 800,000 people worldwide each year as a result of neurological disorders.21
While 69.67% of the stroke patients included in the study were in the dysphagia group, it was noted that the results found in the literature were heterogeneous and generally ranged from 42% and 95%.22 In the study conducted by Broadley et al.23, when the dysphagia findings of 149 stroke patients were evaluated, 50% of the patients were classified as dysphagic. This difference may be due to the different sample size of our study and that of Broadley et al.23 In the study by Tuncay et al.24, it was determined that 50 stroke patients who were fed orally were divided into two groups according to their dysphagia status, and the degree of stroke was higher in the dysphagia group. In this case, it can be said that the severity of dysphagia is closely related to the severity of the neurological disease.24
While 80% of the Parkinson’s patients included in the study were in the dysphagia group, it has been reported in the literature that more than 80% of Parkinson’s patients may develop dysphagia during the course of the disease.25 The basal ganglia, which modulate sensory information, provide a response according to the consistency and texture of the bolus. The high rate of dysphagia in Parkinson’s disease, which is a disease of the basal ganglia, is not surprising.
While 60.8% of MS patients are in the dysphagia group, the literature has shown that this rate varies between 38% and 81%.26 While the rate of dysphagia we found in patients with dementia was 83.32%, the estimated frequency of dysphagia in patients with dementia in the literature varied from 7% to 87%.27 While 60% of patients with CP have dysphagia, the literature suggests that the rate may be as high as 30-40%.28 44.4% of GBS patients and 100% of MG patients were in the dysphagia. The literature suggest that dysphagia may occur in approximately 36% of patients with inflammatory myopathy.8 When comparing the rates obtained, it is possible to see differences due to the size of the sample and the difference in the assessment tool used.
In our study, the item that received the highest score according to the questions of the survey was the item “I have difficulty swallowing solid foods.” In the literature, in the study conducted by Bisch et al.29 in healthy subjects and stroke patients, it was investigated that as the viscosity of the swallowed substance increases, oropharyngeal swallowing efficiency decreases. This was associated with increased viscosity, prolonged oral transit time and prolonged cricopharyngeal patency.29 This may have been influenced by the fact that the participants in our study gave high scores to this item.
In general, the study found that women had a statistically significantly higher rate of dysphagia than men. On the other hand, people aged 65 and over were significantly more likely to have dysphagia. In the literature, an American study found that people who presented to the hospital with swallowing problems during the year were more likely to be female than male. In addition, the same study found that dysphagia was associated with increasing age, which supports the findings of our study.30 In the study by Güçmen et al., stroke patients were divided into two groups, with and without according to the EAT-10 scale.31 While a statistically significant difference was observed between the two groups according to the parameter of age, no statistically significant difference was observed between gender, stroke duration, and BMI.31 The results of the study support our research except for the parameter of gender.
There are no studies that have used objective tests and biomechanical analysis to investigate the factors that vary by gender and iron deficiency which is one of the predictors of dysphagia. However there are also studies that show a statistically significant relationship between gender and iron deficiency, which is one of the predictors of dysphagia. In a study analysing the prevalence of iron deficiency in adult patients, it was found to be statistically significantly higher in women. The higher prevalence of iron deficiency in women may be an effective factor in the higher prevalence of dysphagia in women.32 In addition, sarcopenia has been associated with dysphagia in the literature. Sarcopenic dysphagia is known as dysphagia resulting from sarcopenia of the whole body and the muscles involved in swallowing.33 Sarcopenia is more common in women and in older age.34 The reason why dysphagia was more common in women in our study may be related to sarcopenia.
Anatomical and physiological problems that develop with age can cause dysphagia. Examples include myosin loss and postural changes that occur over time.32 The difference in dysphagia between age groups observed in the study is consistent with the literature. Ageing can adversely affect the oral, pharyngeal, and oesophageal phases of swallowing. This may increase the potential for dysphagia in the future. It is estimated by the 2050s, people over the age of 65 will make up approximately 25% of the population in developed countries.32 This will have an impact on health services.
Dysphagia, which has been associated with aspiration bronchopneumonia and malnutrition in the literature, was not found to be significantly associated with pneumonia and body mass index in our study. This may be due to the fact that the severity of dysphagia in the patients included in the study was not high. In our study, dysphagic patients were not grouped according to the severity of dysphagia. However, the fact that the patients included in the study were fed orally suggests that the severity of dysphagia was not high.
Limitations
During our study, due to the fact that invasive tests were not allowed under pandemic conditions and there was no equipped equipment support, objective dysphagia assessment tests other than the Eat-10 test could not be used. The fact that instrumental tests such as fiberoptic endoscopy and videofluoroscopy were not used is one of the limitations of our study. Studies using objective test will contribute to the literature.
In addition, the inability to distinguish dysphagia from oral, pharyngeal, and oesophageal dysphagia is one of the limitations of our study. Screening with objective tests will contribute to the literature in this direction.
Our study was conducted at a time when it was difficult to conduct research in the hospital under pandemic conditions. The assessment tool we were able to obtain permission to use for the study was the Turkish EAT-10 test. Only people who volunteered to take part and who could experience swallowing in a way that was appropriate to the nature of the test could be included in this test. However, patients from whom we could not obtain consent due to their level of consciousness and patients receiving enteral nutrition, most of whom were in intensive care, could not be included in the study. This situation is the main limitation of our study. Future studies can be extended by including patients with severe dysphagia who were receiving enteral nutrition, using the records of all patient in the hospital.
The hospital was very busy with patients under pandemic conditions. Malnutrition monitoring could not be carried out because there were no suitable conditions for long-term follow-up of participants. Studies comparing the first test and last test and monitoring malnutrition will contribute to the literature.
Ethical approval
This study has been approved by the Non-invasive Ethics Committee of Dicle University (approval date DD.MM.14.04.2022, number 301). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Chen YC, Chen PY, Wang YC, Wang TG, Han DS. Decreased swallowing function in the sarcopenic elderly without clinical dysphagia: a cross-sectional study. BMC Geriatr. 2020;20:419. https://doi.org/10.1186/s12877-020-01832-0
- Sayaca Ç. Investigation the effect of proprioceptive neuromuscular facilitation technique in the rehabilitation of swallowing disorders [dissertation]. Ankara: Hacettepe University; 2018.
- Zevallos JP. International head and neck cancer epidemiology consortium: Update no. 16. Head Neck. 2014;36(10):1391. https://doi.org/10.1002/hed.23845
- Hall JE. Guyton and Hall Textbook of Medical Physiology. 13th ed. Philadelphia: Elsevier; 2016.
- Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018;10:CD000323. https://doi.org/10.1002/14651858.CD000323.pub3
- Feng MC, Lin YC, Chang YH, et al. The Mortality and the Risk of Aspiration Pneumonia Related with Dysphagia in Stroke Patients. J Stroke Cerebrovasc Dis. 2019;28:1381-1387. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.02.011
- Gandhi P, Steele CM. Effectiveness of Interventions for Dysphagia in Parkinson Disease: A Systematic Review. Am J Speech Lang Pathol. 2022;31:463-485. https://doi.org/10.1044/2021_AJSLP-21-00145
- Stathopoulos P, Dalakas MC. Autoimmune Neurogenic Dysphagia. Dysphagia. 2022;37:473-487. https://doi.org/10.1007/s00455-021-10338-9
- Kalatzi M. Standardization and cultural adaptation of the Greek questionnaire for recording dysphagia phenomena in patients with multiple sclerosis (DYMUS) [master's thesis]. Macedonia: University of Macedonia, Department of Educational and Social Policy; 2018. Available at: https://dspace.lib.uom.gr/bitstream/2159/22018/3/KalaitziMariaMsc2018.pdf
- Ejraeı N, Yildiz Ozer A. Trunk Stabilization and Its Rehabilitative Effects in Children with Cerebral Palsy. Abant Tıp Dergisi. 2022;11:123-131. https://doi.org/10.47493/abantmedj.957341
- Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287-298. https://doi.org/10.2147/CIA.S23404
- Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919-924. https://doi.org/10.1177/000348940811701210
- Demir N, Serel Arslan S, İnal Ö, Karaduman AA. Reliability and Validity of the Turkish Eating Assessment Tool (T-EAT-10). Dysphagia. 2016;31:644-649. https://doi.org/10.1007/s00455-016-9723-9
- Schindler A, de Fátima Lago Alvite M, Robles-Rodriguez WG, Barcons N, Clavé P. History and Science behind the Eating Assessment Tool-10 (Eat-10): Lessons Learned. J Nutr Health Aging. 2023;27:597-606. https://doi.org/10.1007/s12603-023-1950-9
- Shimizu A, Fujishima I, Maeda K, et al. Effect of low tongue pressure on nutritional status and improvement of swallowing function in sarcopenic dysphagia. Nutrition. 2021;90:111295. https://doi.org/10.1016/j.nut.2021.111295
- Ulukavak Çiftçi T, Mollarecep ER, Ekim N. Aspiration Pneumonia (Report of Seven Cases and a Review of the Literature). Turk Thorac J. 2004;5:100-105.
- Arrese LC, Carrau R, Plowman EK. Relationship Between the Eating Assessment Tool-10 and Objective Clinical Ratings of Swallowing Function in Individuals with Head and Neck Cancer. Dysphagia. 2017;32:83-89. https://doi.org/10.1007/s00455-016-9741-7
- Ersöz Ünlü EC, Akın Öçal FC. Can Eating Assessment Tool (EAT-10) Anticipate Objective Findings of Dysphagia Patients? Kulak Burun Boğaz ve Baş Boyun Cerrahisi Dergisi. 2020;28:146-151. https://doi.org/10.24179/kbbbbc.2020-75224
- ndrade PA, Santos CAD, Firmino HH, Rosa COB. The importance of dysphagia screening and nutritional assessment in hospitalized patients. Einstein (Sao Paulo). 2018;16:eAO4189. https://doi.org/10.1590/s1679-45082018ao4189
- Abdulmassih EMS, Macedo Filho ED, Santos RS, Jurkiewicz AL. Evolution of Patients with Oropharyngeal Dysphasia in Hospital Environment. Int Arch Otorhinolaryngol. 2009;13:55-62.
- Panebianco M, Marchese-Ragona R, Masiero S, Restivo DA. Dysphagia in neurological diseases: a literature review. Neurol Sci. 2020;41:3067-3073. https://doi.org/10.1007/s10072-020-04495-2
- Banda KJ, Chu H, Kang XL, et al. Prevalence of dysphagia and risk of pneumonia and mortality in acute stroke patients: a meta-analysis. BMC Geriatr. 2022;22:420. https://doi.org/10.1186/s12877-022-02960-5
- Broadley S, Cheek A, Salonikis S, et al. Predicting prolonged dysphagia in acute stroke: the Royal Adelaide Prognostic Index for Dysphagic Stroke (RAPIDS). Dysphagia. 2005;20:303-310. https://doi.org/10.1007/s00455-005-0032-y
- Tuncay F, Taşbaş Ö, Borman P, Geçene M, Coşkun Ö. The Bedside Clinical Evaluation of Swallowing Function of Stroke Patients in Acute Stage. J PMR Sci. 2011;14:33-38.
- Suttrup I, Warnecke T. Dysphagia in Parkinson's Disease. Dysphagia. 2016;31:24-32. https://doi.org/10.1007/s00455-015-9671-9
- Ansari NN, Tarameshlu M, Ghelichi L. Dysphagia In Multiple Sclerosis Patients: Diagnostic And Evaluation Strategies. Degener Neurol Neuromuscul Dis. 2020;10:15-28. https://doi.org/10.2147/DNND.S198659
- Wang S, Gustafson S, Deckelman C, et al. Dysphagia Profiles Among Inpatients with Dementia Referred for Swallow Evaluation. J Alzheimers Dis. 2022;89:351-358. https://doi.org/10.3233/JAD-220402
- García Ron A, González Toboso RM, Bote Gascón M, de Santos MT, Vecino R, Bodas Pinedo A. Nutritional status and prevalence of dysphagia in cerebral palsy: usefulness of the Eating and Drinking Ability Classification System scale and correlation with the degree of motor impairment according to the Gross Motor Function Classification System. Neurologia (Engl Ed). 2023;38:35-40. https://doi.org/10.1016/j.nrleng.2019.12.006
- Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL. Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Hear Res. 1994;37:1041-1059. https://doi.org/10.1044/jshr.3705.1041
- Bhattacharyya N. The prevalence of dysphagia among adults in the United States. Otolaryngol Head Neck Surg. 2014;151:765-769. https://doi.org/10.1177/0194599814549156
- Güçmen N, Güçmen B, Koca TT. The Importance of Malnutrition and Dysphage in Patient With Stroke. Kahramanmaraş Sütçü İmam Üniversitesi Tıp Fakültesi Dergisi. 2022;17:182-190. https://doi.org/10.17517/ksutfd.876155
- Karakuş V, Giden A, Ersil Soysal D, Bozkurt S, Kurtoğlu E. Evaluation of Anemia in Terms of Etiology, Risk Factors, and Relaps in Adult Patients. Medical Journal of Mugla Sitki Kocman University. 2016;3:1-6.
- Fujishima I, Fujiu-Kurachi M, Arai H, et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatr Gerontol Int. 2019;19:91-97. https://doi.org/10.1111/ggi.13591
- Sökmen ÜN, Dişçigil G. Sarcopenia in the elderly. The Journal of Turkish Family Physician. 2017;8:49-54. https://doi.org/10.15511/tjtfp.17.00249
Copyright and license
Copyright © 2025 The author(s). This is an open-access article under the terms of the Creative Commons Attribution License (CC BY) which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.